Allergic Rhinitis & Sinusitis
Require definitive diagnosis due to overlapping symptoms

Case Study 1 :
Question: My son was 7 years old this year. He suffered from sinusitis which caused headache for nearly a year. Although the doctor gave nasal spray, his situation did not improve so far. May I know how to solve this problem?
First of all, doctor must determine whether it is allergic rhinitis or sinusitis, because these 2 diseases are showing similar symptoms that sometimes overlapping with each other. Therefore, a detailed investigation is required.
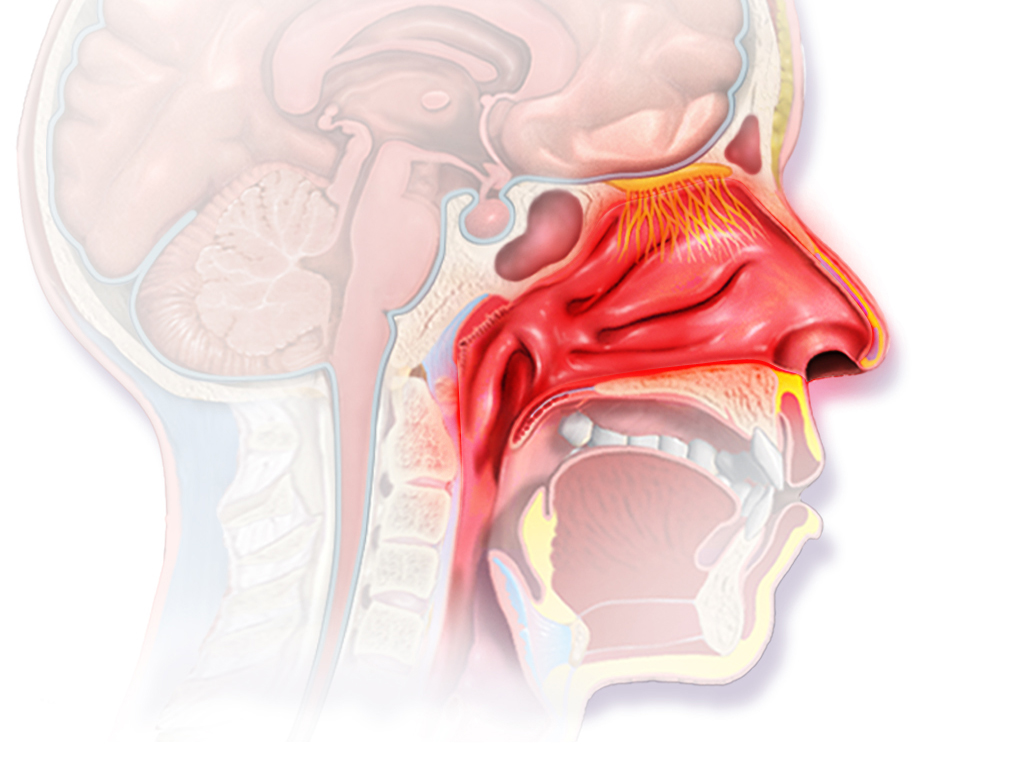
Allergic rhinitis: As the name implies, nasal allergies caused by the environment, allergens, heredity that triggering inflammation of the nasal mucosa. If the condition persists, it can lead to sinusitis. Symptoms include itchy nose, red eyes, runny nose (clear fluids), stuffy nose, sneezing, etc. The symptoms can be treated by the following methods:
- Anti-histamines to reduce nasal secretion
- Nasal cavity cleaning
- Nasal steroid sprayer

Sinusitis: The sinuses are in the cavity of the facial bone near the eyes and nasopharyngeal cavity, filled with air and communicated with the nasal cavity. Sinusitis generally refers to inflammation of the sinuses. The inflammatory reaction can cause swelling of the nasal mucosa, increase of nasal secretions, and obstruction of the sinus ostium, which makes the bacteria more susceptible to growth and reproduction. Symptoms of sinusitis include persistent nasal discharge, yellowish green colour, chronic nasal obstruction, increased nasal secretions, and coughing, especially when sleeping and waking up. Sinusitis also causes odour during exhalation, and headache.
Question: Will doctors encourage surgery?
In general, if children have sinusitis, headache or dizziness does present normally. Parents should take their children to the paediatric department for doing detailed examination. Functional intranasal examinations are usually performed first in the Otorhinolaryngology department. If necessary, an imaging procedure such as sinus X-ray or CT Para sinuses is performed.
Acute sinusitis is usually accompanied by fever, treatment options include antibiotics, analgesics, anti-histamines, nasal cleansing, and use of intranasal nebulizers.
In severe cases, maxillary antral washout can be used to drain the pus and inject anti-inflammatory drugs. The treatment of chronic sinusitis is similar to allergic rhinitis. If there are nasal polyps, middle turbinate hypertrophy, nasal septum deviation, etc. then surgical treatment may become an option to be considered by patient.
Cold, dusty, and constant nasal rhinitis or
allergies and vasomotor rhinitis
Case Study 2 :
I have faced rhinitis problems since childhood. Every time weather turns cold, I will continue to sneeze and experience runny nose. However, after a while it will become ok, so I’m used to it.
In recent years, the problem of rhinitis seems to get worse. I will sneeze and experience runny noses almost every morning. It becomes fine again when weather is back to warmer condition. However, there are often nasal discharges that flowing into throat, causing throat problems, hoarseness, and frequent sore throats. Especially when I wake up in the middle of the night or get up in the morning, I feel dryness and tingling in my throat. I need to drink some water to ease such discomforts.
A few days ago, when I was doing some house works, inevitably I inhaled a lot of dusts, and experienced sneezing and runny nose, thereafter I felt sore throat. The symptoms lasted for two or three days. This kind of situation improved quickly in the past, but this time it continued for longer while. It’s really bothered me.

Question: Why rhinitis happens? Is it related to our eating habits?
Is there any way to improve my condition?
The symptoms you described likely related to syndrome of allergic rhinitis and vasomotor rhinitis.
The reason of allergic rhinitis is because of the patient’s exposure to allergens. Common allergens – mites found in bedding sheets, pet hair and dander, plant pollen, or certain foods.
Vasomotor rhinitis is caused by changes of ambient air temperature (e.g., relatively its symptoms are more severe in the colder morning. Once the weather turns warmer in the middle of the day, the situation can get much better), emotional factors, or exposure to certain irritating odours (caused by perfume, cigarettes, lacquer, alcohol, or spicy food.
Both allergic rhinitis and vasomotor rhinitis are showing similar symptoms, including runny nose, stuffy nose, sneezing, etc. When the condition of patient deteriorates, there will be a situation where the nose drips (flowing from the nose to the throat), causing nasal discharge enters the throat, end up resulting discomfort, coughing, itching in the throat, and even inflammation of the throat. At the same time, no thanks to stuffy nose, patients habitually use mouth breathing during sleep, of which it can trigger dry throat and discomfort.
In terms of treatment, patients must pay attention to their home and work environments, in order to avoid the exposures of allergens or irritating factors that cause rhinitis:
- Wash bed sheets and sheets from time to time (recommended to wash once a week) and soak in hot water for several minutes to remove mites.
- Avoid adjusting the air conditioner temperature to too low level
- Try to use less detergent
- If the work environment cannot avoid smoke, chemical gases or dust, then patients must wear a protective mask.
- As far as foods are concerned, apart from avoiding spicy foods, if patients know they are sensitive to certain foods, they must avoid them as much as possible.

At present, some government hospitals (including the Otorhinolaryngology Department of University Malaya Medical Centre) have started offering allergy testing services that can make patients more aware of their allergens, including what types of food causing their allergies.
If symptoms do not improve after patients have changed their lifestyle, they will have to rely on drugs to control their conditions. Of course, it is recommended that doctor must make definite diagnosis prior to using any medicines. Commonly used drugs include oral anti-histamines, nasal decongestants and intranasal steroid sprays.





